
Valerie Henderson
2020. Central Oregon Community College. Bend, Oregon
I have always viewed massage therapy as a form of self care that can foster both emotional and physical healing. Self care is more important now than ever, and I am so excited to be able to positively impact the lives of others. I plan on using this scholarship to further my education (hopefully becoming certified in the Graston Technique) and start a sports medicine-focused career. We all need connection and joy in our lives, and I cannot think of a better medium to encourage this than massage therapy.
Piriformis Syndrome:
Symptoms, Causes and Lifestyle Implications
by Valerie Henderson
28 February 2020
Understanding the Pelvis
Anyone who glances at the pelvic girdle anatomy would agree that there is a lot going on. Some of the largest and most powerful muscles in our body attach to our ilium, ischium and pubis – our “hip bones” – including the gluteal muscles, hamstrings and quadriceps groups. To simplify, the hips are responsible for the initiation of leg movement, as well as supporting the weight of our bodies. Our hips create a ‘hinge’ in the middle of our bodies, allowing for countless activities. They also play a significant role in our proprioception abilities (this deals with how aware we are of our bodies’ positioning in space). Walking, running, sitting, dancing, standing upright… the list of activities that require hip movement is endless. Understanding the hips can be the key to effectively helping any client with hip issues or pain.
As with any ball-and-socket joint, the acetabulofemoral joint consists of a rounded, hollow socket (the acetabulum of the hip) and a ball-like structure that rests in that hollow (the head of the femur). This design is intended to produce rotational movements that are fluid in all directions. What guides and controls these movements? The surrounding muscles, of course!
Piriformis Syndrome: A (Literal) Pain in the Butt
While watching a soccer match or a track meet, most of our recognition goes towards the explosive movements generated from the gluteus maximus. But what about those smaller, precise movements? Not all of the credit can go towards the larger, more pronounced muscles. To move efficiently, our hips should be able to rotate internally and externally. Doing so ensures that the muscles in our trunk and lower legs are not being over-utilized. If there is too much tightness or laxity in our internal or external rotators, other muscles can take on too much work. This can easily lead to overuse injuries and muscular imbalances.
Hidden deep underneath the superficial gluteus maximus lies the piriformis muscle. Originating at the sacrum and inserting at the greater trochanter, the piriformis muscle is one of six muscles (sometimes known as the “deep six”) responsible for externally rotating the hip. The very name describes the shape – in Latin, piriformis roughly translates to “pear shaped.” If functioning normally, the piriformis assists in external rotation and abduction of the hip (specifically, while the hip is in flexion). It is worth noting that the piriformis muscle lies very closely to the largest nerve in the body – the sciatic nerve. All of the lateral rotators lie deep to the sciatic nerve, except the piriformis. Its positioning and proximity to this nerve is where a sleuth of problems can arise.
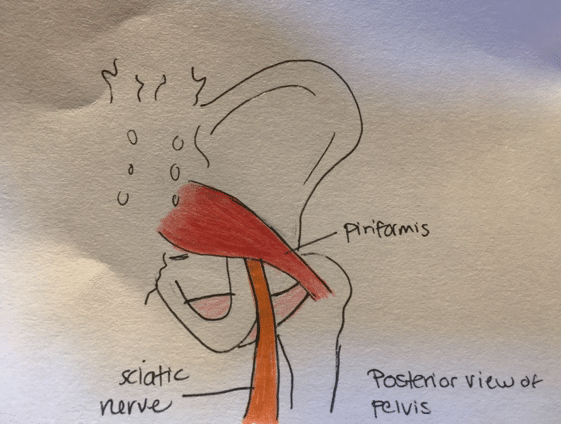
During palpation, the piriformis is a standout muscle compared to the deeper lying lateral rotators (such as the obturator internus). Its superficiality can also be the culprit for sciatic issues. Because the sciatic nerve is sandwiched between the piriformis and the five other external rotators, over-contraction of the piriformis can compress the sciatic nerve. This phenomenon is commonly referred to as “piriformis syndrome” and can be as troubling to diagnose as it can be to treat. This syndrome has many symptoms. Most commonly, an individual can expect to feel:
- Dull, relentless aching in one buttock
- Limited range of motion in the affected leg
- Sciatica (pain radiating down the posterior leg, calf, and foot. May also manifest as a numbing, pins-and-needles sensation)
- Pain during prolonged sitting
- Sharp or dull pain in middle of buttocks when walking or running on a non-flat surface
- Poor balance when standing on one foot
- In rare cases, bowel movements may be painful
In a clinical setting, larger muscle groups such as the hamstrings or quadriceps are often examined first to ensure these symptoms cannot be attributed to tightness or weakness in these areas. While there is not a single test used to diagnose this syndrome, a clinician may use specific modalities on the client in an attempt to re-create the pain associated with piriformis syndrome. Usually, this would include range of motion exercises, as well as a physical examination. The client’s description of their own symptoms can be reliable as well.
In some cases, piriformis syndrome may be difficult to diagnose. Its symptoms can closely resemble a condition known as lumbar radiculopathy. Both conditions are caused by nerve compression, but the difference lies in where the compression is occurring.
Etiology
As was previously mentioned, an over-active piriformis muscle is usually the culprit for sciatic nerve impingement or compression. But what causes this muscle to become irritated in the first place? Unfortunately, the answer can vary from person to affected person. In some individuals, piriformis syndrome can be attributed to a packed wallet that is carried in the back pocket of their pants. Sitting down with an over-stuffed wallet causes the ischial tuberosities, or “sitting bones” to be elevated on one side. This instability, paired with the added pressure of the wallet sitting right against the piriformis, puts extra pressure on the sciatic nerve. These individuals are said to suffer from “fat wallet syndrome”; a more colloquial term for piriformis syndrome.

For others, activity level can be the culprit of piriformis pain. Overtraining in many endurance sports (such as long distance running or hiking) can lead to an over-utilized piriformis muscle. Oftentimes, self-proclaimed “couch potatoes” will make quick and drastic changes to their activity levels. The sudden change from a sedentary lifestyle to one filled with movement can be enough to cause irritation in the piriformis, as well as other surrounding muscles. Overuse injuries and fat wallet syndrome are examples of microtraumas – a smaller trauma caused by repetitive overuse over time. Macrotraumas, on the other hand, are characterized by a single event that that leads to major trauma. Examples of this include a car accident, bone fractures, or a joint dislocation. Piriformis syndrome can occur from a direct fall or impact to the buttocks.
Genetics should not be overlooked when examining the piriformis. Women are found to suffer from piriformis syndrome far more frequently than men. The exact reasons are still not known, but it is believed to be attributed to the pelvic differences between men and women. The female pelvis is biomechanically different than that of the male pelvis. In women, the quadriceps femoris muscle pulls more laterally on the patella (kneecap) than it does on the male pelvis. This creates a wider quadriceps angle, more commonly referred to as the “Q angle.” Additionally, the childbearing capabilities of women yield a wider pelvis. This wider Q angle can lead to excessive medial rotation of the femur. Over time, this can put extra stress on the piriformis muscle and the sciatic nerve.

Implications on Lifestyle
After studying the many causes of piriformis abnormalities, it begs the question: what can be done to treat such a fickle condition? The answer usually lies in the cause itself. Cortisone injections and pain medications can provide temporary relief from the inflammation but may only serve as a bandage. Treating the root cause often requires a lifestyle change from the individual. Sometimes, a person suffering from piriformis syndrome can develop an antalgic gait. This is a gait that develops as a means to avoid pain when walking. Physical therapy can be intensely helpful in retraining a person’s gait, as well as strengthening surrounding muscles.
Physical therapy may or may not be accompanied by a period of rest, in which the individual should refrain from the activity that contributed to piriformis syndrome. To avoid re-injury, returning to these activities should be done gradually and with the guidance of a physician or medical professional.
Massage therapy in particular has been cited as a great way of relieving piriformis syndrome pain. It is important that the massage therapist be educated on trigger point therapy, as well as the specific referred pain patterns with this condition. Once the root cause of the individual’s pain has been addressed, massage has been found to be an excellent way of managing (and, in many cases, eliminating) lingering pain from this debilitating condition.
The world of healthcare is constantly evolving and expanding. While our approach to treatment is based on what we currently know, it should always be punctuated with curiosity. At the end of the day, new breakthroughs in medicine and healthcare can be accredited to our desire to grow and nurture the human condition. Ask yourself: what has yet to be explored?
Sources
Biel, Andrew. Trail Guide to the Body: a Hands-on Guide to Locating Muscles, Bones and More. Books of Discovery, 2014.
Boyajian-O’Neill, Lori A., et al. “Diagnosis and Management of Piriformis Syndrome: An Osteopathic Approach.” The Journal of the American Osteopathic Association, American Osteopathic Association, 1 Nov. 2008, jaoa.org/article.aspx?articleid=2093614.
(All images were hand-drawn by myself)